The state of North Carolina expanded Medicaid eligibility starting on December 1st, 2023. The state passed enabling legislation this summer to accept the Affordable Care Act’s (ACA) enhanced funding to provide health insurance to working-age adults who are:
- US citizens or qualified immigrants
- Between the ages of 19 and 64 and
- who earn under 138% Federal Poverty Level(FPL) (<$20,120 for a single individual) without any other asset or work requirements.
North Carolina is the 41st state to expand Medicaid eligibility. The state anticipates covering over 600,000 adults with this program.
I am working towards my doctorate in Health Services Research with a policy focus. I am fundamentally fascinated by insurance markets, consumer choice and the navigation of complex choice environments.
So what do we need to know?
The North Carolina Department of Health and Human Services (DHHS) provides a convenient guide:
- The best way to apply is online through ePASS; you can also apply in-person, by phone or mailed applications. The processing time for applications can be up to 45 days. Applications submitted online may be processed faster.
- The coverage will be comprehensive, including services like primary care, hospital stays, maternity care, vision and hearing, dental/oral health care and more.
- Medicaid pays for doctor visits, yearly check-ups, emergency care, mental health and more – at little or no cost to you.
- Current beneficiaries with full Medicaid coverage will not see any changes.
If you currently have full benefit Medicaid, nothing will change for you. If you have recently lost coverage due to benefit redetermination, you should re-apply for coverage on or after December 1st as the eligibility criteria will be dramatically more expansive and easier to qualify for than today. If you have Family Planning limited benefit Medicaid, you will be automatically enrolled if you are income eligible into Medicaid Expansion effective December 1st. This is the case for nearly 1,990 Orange County residents, according to a recent presentation by the Orange County Department of Social Services.
Where can I get questions about Medicaid answered in Orange County?
Orange County Department of Social Services is the local Medicaid eligibility determination agency. They can help you complete your application and answer questions that you may have. (They recently hired nine new employees in anticipation of this change.) Medicaid coverage is retroactive for up to 3 months after the application date OR program start date. So if you apply in mid-December, Medicaid will (eventually) pay for a doctor’s appointment or a hospital visit that occurred on December 1st. If you only qualify for Medicaid Expansion, you likely will not have a bill paid if you incurred the service before December 1st.
What do I do if I am income-eligible for Medicaid but already purchased an ACA plan on healthcare.gov or through a broker?
The ACA provides premium subsidies to qualified individuals to help them pay the monthly fee for insurance. Qualified individuals are US citizens or qualified immigrants with incomes of at least 100% FPL and have no other eligibility for other health insurance coverage.
Healthcare.gov, the federal enrollment platform for the ACA, runs an eligibility for Medicaid check based on age and income. If there is a prima facie reason for Healthcare.gov to believe that you’re eligible for a state Medicaid program on the day that you update your account, Healthcare.gov pauses your subsidy eligibility and sends you to the state Medicaid agency for an eligibility determination.
This means that if you currently have a plan that you actively selected in November with the intent that the plan starts on January 1, 2024, you will stay in that plan. If you go online to pick a plan on or after December 1st you will have a Medicaid eligibility check conducted before you’re allowed to pick a plan with premium subsidies. This is really important for people who have plans known as “CSR-94” or “Extra Savings” Silver plans.
The biggest thing with health insurance as I repeatedly tell my students is that this is a confusing and complex decision system. It is okay to ask for help. Lean into Orange County DSS and the community health centers that serve Orange County as these groups will know what is up and how to connect you to the right sort of help.
How many people will this help in Orange County?
The Orange County Department of Social Services recently presented to the county commissioners about the rollout. According to their estimates, that could add more than 5,300 people in Orange County the first year of expansion.
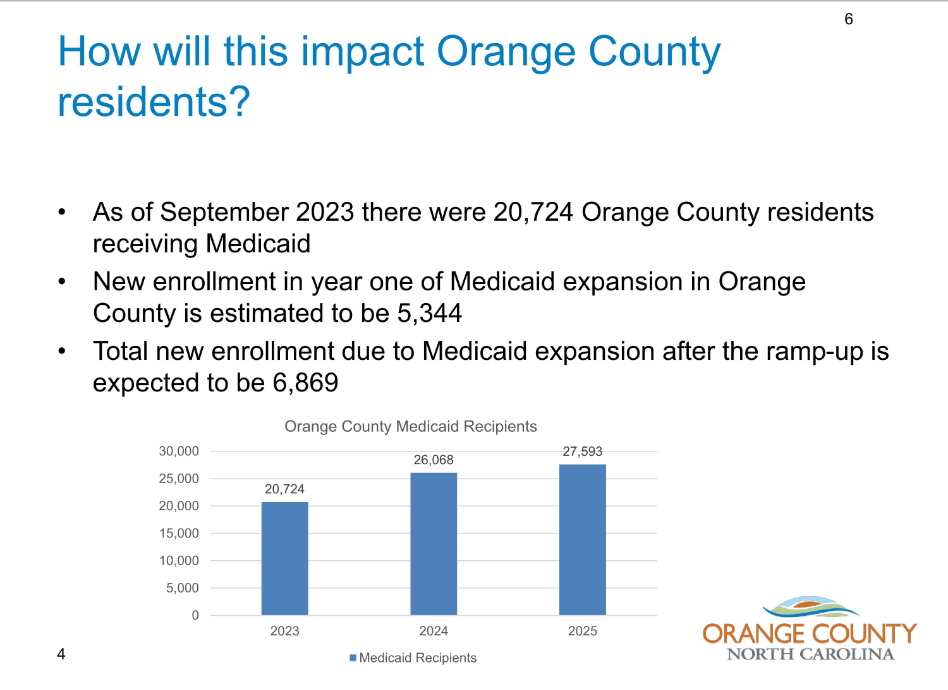
The complete presentation is available here. All of Orange County’s representatives in the state legislature voted in favor of Medicaid expansion last March.